Following is a case study on one of my patients in the Health Center at LCCW. I wrote this for a research class, so once again, it’s pretty techie, but something our field is working on is building our scientific research, so here is my first contribution. Enjoy!
Case Study: Non-specific Low Back Pain: A Quick Response to Chiropractic Care
Abstract
OBJECTIVE: To show the outcome of chiropractic care for a patient with lumbalgia while exercising.
CLINCIAL FEATURES: The patient was a 28-year-old woman who presented with complaints of low back pain while exercising. Aberrant spinal biomechanics and fixation of joints were diagnosed from physical exam findings. Prior to care she had taken over the counter anti-inflammatory medications to alleviate pain along with having positive previous results from chiropractic care.
OUTCOMES MEASURES: Changes in this case were measured through thorough static and motion palpation findings to detect change in spinal biomechanics.
INTERVENTION AND OUTCOME: Diversified chiropractic care was delivered to areas of the pelvis and lumbar spine that displayed decreased range of motion and fixation of joints. Throughout the course of 11 chiropractic adjustments, the symptoms resolved completely allowing the patient to return to her normal activities. Continued adjunctive care has helped this patient remain pain free.
CONCLUSION: This case report illustrates that patients presenting with non-specific low back pain benefit from chiropractic care. Further research in this area would benefit the large population of people who suffer daily from lumbalgia.
Introduction
Low back pain, also known as Lumbalgia, is a common complaint among people all over the world. In the United States this condition is often seen as a serious public health concern because of its effects on occupational productivity, resulting in financial costs as well as social costs.1 According to Balague, et al, “most people will experience back pain at some point in their life” yet few, less than one third, will seek care. 2 They refer to people of all ages from adolescents to the elderly predominantly affecting those aged 35-55. The CDC reports industrialized nations can expect an estimated prevalence of 70%3 and a 2012 study showed that just over one quarter of adults, of both genders, had experienced low back pain in the previous 3 months and 55% had the experience in the last year.4
A definition of low back pain must also be considered as some cases are mild while some are severe. Mild cases are often labeled acute in which the duration of pain is under 3 months and more severe cases are considered chronic in nature lasting longer than 3 months.5 It is important to note that those who suffer from acute cases may also experience recurrent episodes of low back pain throughout life.
Because it is subjective, a patient presenting with a history of lumbalgia is often enough to diagnose the condition. Within the chiropractic field however, orthopedic exams are used to determine more specificity as to what is actually causing the pain in the low back region, differentiating it from pain generated from the pelvis. According to Lehman, it is imperative to be able to differentiate normal spinal biomechanics for a proper diagnosis of low back dysfunction. He states, “A diagnosis based on function via tools and techniques to quantify dysfunction provides a means to assess a patient’s current condition separate from their subjective perception of pain.”6 The authors of The Burden of Musculoskeletal Diseases show disc degeneration is the most common low back diagnosis, which is directly related to aging, an alter in spinal biomechanics, and a recent correlation with genetics.7
Traditional treatment of non-specific back pain consists of over the counter NSAIDs, pharmacotherapy and physical therapy, and surgical intervention as deemed necessary for those with progressed neurological symptoms or deficits. Complementary Alternative Medicine (CAM) is often considered for those who do not choose to address their condition with traditional medical treatment. In many cases, those patients who have already tried “everything else” approach CAM. This often includes massage, acupuncture, and spinal manipulation in the form of specific chiropractic care.
Low back pain is one of the most costly conditions in the US with a reported estimate of $84.1 billion to $624.8 billion in direct and indirect costs, including loss of work, as well as being “the second most common reason for visits to physicians”.4
Low back pain is, more often than not, a complaint of the musculoskeletal system along with the nervous system. Both of these are addressed specifically by chiropractic through the use of high velocity, low amplitude spinal adjustments. “Chiropractic doctors typically serve as portal of entry providers focused primarily, although not exclusively, on neuromusculoskeletal disorders.”8 Because of the conservative, hands on approach that chiropractic takes on low back pain with an emphasis on patient education, exercise, diet and lifestyle recommendations, they generally help patients get well faster than an allopathic approach. In an article evaluating chiropractic management for low back disorders a group of chiropractors managed low back cases with similar evaluations, treatment plans and reevaluations, paying particular attention to red flags. The group came to 80% consensus that this specific care was best for patients with low back pain.8
Case Report
A 28-year-old female patient presented with a primary complaint of low back pain, typically occurring 2-3 times per week while she was on a regular work out schedule of cardio exercise and weight lifting 5-6 days a week. The low back pain, which began in 2008, was insidious in onset and related to stress. She reported the pain was located in her lumbo-sacral area and “moved around” to her flanks. The pain was worsened through too much working out, dancing, or occasionally sleeping in the wrong position. Usually this pain lasted 4-5 hours, but sometimes was reported to remain constant throughout the entire day, even waking her up at night. The patient reported a VAS of 5/10 and 9-10/10 when at its worst. The patient reported her activities of daily living were limited, directly impacting her ability to participate in recreation without pain, as clearly illustrated through a GPDIQ score of 3. She reported a previous positive experience with chiropractic, earlier in the year.
The physical exam revealed abnormal posture in which the right ilium was slightly higher than the left. The lumbar active range of motion was limited in bilateral lateral flexion at 25/30 degrees as well as being limited in bilateral rotation at 25/30 degrees. Palpation revealed slight edema and hypertonic multifidus and quadratus lumborum musculature bilaterally from L3 to both SI joints. Muscle strength testing revealed a slight decrease in strength of the left psoas. The Prone Leg Check was positive on the right and ¼” short. The Supine Leg Check was positive on the left and ¼” short. Standing Gillet’s test revealed a fixated right ilium with bilateral cavitation during sacral motion. Kemp’s test on the right was negative for disc involvement yet produced left sided low back muscle pulling indicating local spastic musculature and possible facet involvement. Yeomen’s test on the right sacroiliac joint revealed decreased ROM with no reported pain indicating fixation of the right sacroiliac joint.
Evaluation of radiographs showed knife clasp deformity at L5/S1. Though suspected, there were no degenerative changes revealed in the lumbo-pelvic region. Motion palpation of L3 found misalignment and fixation to the right. Motion palpation revealed fixation of the right ilium posterior inferior.
The clinical impression was chronic moderate to severe frequent lumbalgia.
Intervention
After the patient had been properly examined and assessed for subluxation through static visualization for asymmetry in posture, static palpation for tonal changes in the tissues and motion palpation to detect fixation and restricted range of motion in the spine and pelvis,
chiropractic care began with adjustments to correct the posterior inferior right ilium. The procedure was to place the patient with her left side down in side posture position squaring the shoulders and hips on the diversified adjusting bench to remove any potential rotation.9 The doctor brings the upside hip and leg into flexion taking the joint to tension with their contact hand and delivering a high velocity, low amplitude (HVLA) adjustment through the plane line of the joint. Subsequent visits addressed subluxation of the lumbar spine also in the side posture position with the patient lying on the side contralateral vertebral spinous rotation. All adjustments were delivered manually with a HLVA thrust.
The patient was adjusted 11 times over an 8 week period using Diversified technique as described by Dr. Michael Schmidt in Diversified Technique.9 Adjustments of the right ilium were given on the first and second visits of this study. These adjustments were performed with the subject lying on an adjusting bench on her left side in diversified side posture position. The contact point was the posterior superior iliac spine with the pisiform of the doctors contact hand delivering the force. The doctor was in lancer’s stance supporting the patient and stabilizing the patients’ right shoulder. Adjustments of the 3rd lumbar vertebrae were given on visits three through six, nine and eleven. These adjustments were performed with the subject laying in diversified side posture position on her right side. The doctor was in lancer’s stance supporting the patient and stabilizing the left shoulder with the contact hand’s pisiform contacting the ipsilateral spinous process. Adjustments of the 1st lumbar vertebrae were given on visits seven and eight of the study. These adjustments were performed with the subject lying on her left side on a bench in diversified side posture position. The doctor was in lancer’s stance supporting the patient and stabilizing the right shoulder with the contact hand’s pisiform contacting the ipsilateral spinous process. For each adjustment, the thrust was delivered through the pisiform of the doctors contact hand as the patient was brought over for the proper line of correction.
Following each adjustment the patient was re-assessed by static and motion palpation to verify the adjustment had altered the tone, reduced the fixation and increased the range of motion.
Visits occurred 1 time per week for the first 3 weeks of care, 2 times during the 4th week of care, 1 time per week for 4 weeks and 1 visit for the last week.
Previous experience with this kind of case is limited to 4 other cases this doctor has treated in her short career as a chiropractor. In each of those cases, the patients reported decreased pain and beneficial outcomes.
Outcome
Initially the symptoms the patient reported as lumbo-sacral pain bilaterally into the flanks. The subject described the pain as sharp and sometimes referring up the spine. There were no radicular symptoms reported. Upon the initial visit the Visual Analog Scale (VAS) was a 5/10 and at its worst 9-10/10. The General Pain Disability Index Questionnaire (GPDIQ) was a 3 and activities that aggravated the complaint were: too intense of a work out or hiking or dancing and occasionally sleeping in the wrong position. At the second visit, the patient reported no pain in the low back since the first adjustment. During the third visit the patient reported mild pain, a 1/10 VAS, and that she was asymptomatic for one day, had slept more hours than normal and woke up with a return of low back pain. Upon presentation to care the pain had improved with movement. The patient was asymptomatic for visits four through six. Upon the seventh visit the patient reported a day of cleaning and yard work along with a family visiting and a heavy work out the previous night which caused the low back pain to escalate to a VAS 7/10. At the following visit a VAS 0-3/10 was reported and then she returned to being asymptomatic for the remainder of treatment. At visit ten, the patient was completely clear of lumbar or pelvic subluxation and the patient reported an absence of lumbo-pelvic pain with a VAS 0/10.
Upon the re-evaluation, the patient reported a 99% improvement in low back pain, which only occurred 1-2 times per month lasting 2-3 hours. A 0/10 VAS and 0 GPDIQ was reported. Changes in the patients’ presentation were documented upon re-evaluation exam as follows: the right hip was more level with the floor and there continued to be slight edema bilaterally over the sacro-iliac joints. Range of motion in the lumbar spine increased to a normal range. Psoas muscles that previously had been weak were now strong. The Prone Leg Check revealed even legs. Previous orthopedic tests including Kemp’s, Yeoman’s and Standing Gilet’s (all of which had elicited symptoms or tightness) were negative.
The patient reported, “Chiropractic care has been the best thing that happened to me in the past year.” She has since returned to working out more regularly, but continues to limit the intensity to prevent aggravation of the low back pain. It was recommended that as the patient increases work out load, she return for care every 2 to 3 weeks to help maintain the asymptomatic state.
Discussion
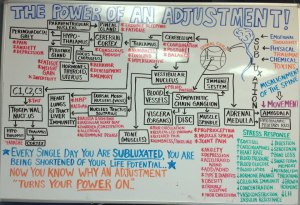
This case is an attempt to describe how chiropractic care for non-specific low back pain can assist one patient’s journey from a symptomatic to an asymptomatic quality of life. The use of HVLA chiropractic adjustments to the fixated segments in the lumbar and pelvic regions of the spine resulted in a consistent decrease in the reported levels of pain while increasing efficacy of spinal biomechanics. The body is a naturally healing entity. There is enough evidence present to demonstrate how spinal manipulation affects the central nervous system causing the brain to “reset” its interpretation of pain and discomfort resulting in substantial relief for the subject. Through the application of HVLA, increased activation of the neuronal afferentation in the muscle spindles is initiated, eventually culminating in a complete summation and silence, at the point of force application. This silence in muscle spindle receptors allows for normal sequencing, recruitment and coactivation of muscles to stabilize and protect the spine as well as return the joint to a normal range of motion and has the potential to decrease pain.10
In accordance with recommended management for non-specific low back pain, Balague, et al, discusses spinal manipulation and treatment of this course as part of most clinical practice guidelines.2 The specific protocol utilized to provide chiropractic care for this patient’s condition was selected based on clinical experience of the researcher, and in accordance with the clinical guidelines of the Health Center at Life Chiropractic College West. This case supports the efficacy of HVLA in the treatment of lumbalgia, as outlined in the studies mentioned above.
During most of this study, the patient had decreased and irregular physical activity causing a decrease in symptomatic presentation. In the middle of the study, an abnormal increase in the amount of physical work occurred, placing increased stress on the subjects low back causing an increase in symptomatology. This is an example of the uncontrollable variability of patient lifestyle. Although core-bracing exercises were recommended as a part of the management plan to help strengthen and protect from further exacerbation of lumbalgia, patient compliance is a large variable and hard to account for. The patient reported successful completion of the exercises, but accuracy cannot be ensured, as the subject was not held responsible for recording the activities on a daily basis. A final limitation is the absence of validation by an external group of researchers. Placebo care was not implemented in this study as it is a case study.
It is well documented that those who suffer from acute cases of low back pain are likely to suffer from recurrent issues.2 An important variable to consider in this study is the relative limited experience of the practitioner performing the care. Although positive results were achieved with regards to the patient’s symptomatic state, it could potentially have been achieved sooner had it been performed by a more experienced chiropractor. This case assists in the confirmation of efficacy for HVLA manipulations as intervention for acute lumbalgia; as also reported by Globe, et al, in which 40 chiropractors reached a high consensus about the specific recommendations for assessing and treating low back disorders.8
Conclusion
This case follows a 28-year-old woman through 8 weeks of chiropractic care to address her complaints of low back pain while exercising. Chiropractic care was provided using Diversified technique for the correction of subluxation in her pelvis and lumbar spine. After the initial phase of care, the patient reported a GPDIQ score of 0 and a reduction and frequency of regular low back pain while exercising. The CDC states the condition of low back pain has a 70% prevalence in industrialized nations.3 This case shows a favorable outcome for this individual, while demonstrating the potential for similar successes for the multitudes of people who suffer from low back pain. However, studies which include a larger sample size, specific guidelines for selecting cases, and appropriate documentation of patient reported treatment plan adherence would help gain substantial evidence of how specific chiropractic spinal manipulations contribute to resolving low back complaints.
References
- The epidemiology of low back pain in primary care. Kent PM, Keating JL. Chiropr Osteopat. 2005 Jul 26;13:13. PubMed PMID: 16045795; PubMed Central PMCID: PMC1208926.
- Non-specific low back pain. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Lancet. 2012 Feb 4;379(9814):482-91. doi: 10.1016/S0140-6736(11)60610-7. Epub 2011 Oct 6. Review.
- http://www.cdc.gov/niosh/docs/97-141/pdfs/97-141.pdf
- The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. Spine (Phila Pa 1976). 2012 May 15;37(11):E668-77.
- Contemporary concepts in Spine Care: spinal manipulation therapy for acute low back pain. Dagenais S, Gay RE, Tricco AC, Freeman MD, Mayer JM. NASS Spine J. 2010 Oct;10(10):918-40.
- Biomechanical assessments of lumbar spinal function. How low back pain sufferers differ from normals. Implications for outcome measures research. Part I: kinematic assessments of lumbar function. Lehman GJ. J Manipulative Physiol Ther. 2004 Jan;27(1):57-62. Review. PubMed PMID: 14739876.
- United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States [Internet]. 2nd edition. Rosemont, IL: American Academy of Orthopedic Surgeons; 2011.[cited 2013 Jan 31]. Available from: http://www.boneandjointburden.org/
- Chiropractic management of low back disorders: report from a consensus process. Globe GA, Morris CE, Whalen WM, Farabaugh RJ, Hawk C; Council on Chiropractic Guidelines and Practice Parameter. J Manipulative Physiol Ther. 2008 Nov-Dec;31(9):651-8. doi: 10.1016/j.jmpt.2008.10.006. Review. PubMed PMID: 19028249.
- Schmidt, Michael J. Diversified Technique. 1990.
- Slosberg, Malik, DC. Subluxation Physiopathology Class Notes, Fall 2012. Pg. 64.
All Material Copyright © 2013 by Ariel Provasoli